First Aid of Choking
Chocking is caused by mechanical obstruction of the airway. The airway can be blocked by vomitus, foods, blood clots or objects. Obstruction of airway can be complete or incomplete. If left for about 5 seconds, patient may die or succumbs severe brain dysfunctions. Chocking is more common in children than in adults with only 20 percent of cases occurring over the age of 15 years. Risk factors for chocking in adults include age over 75 years, neurological disorders, loss of consciousness, and alcohol or sedative use.
Chocking should be suspected in children who have sudden onset of lower respiratory symptoms, or those who do not respond to standard management of other suspected etiologies such as pneumonia, asthma, or croup. The risk is highest in children between one and three years of age.
A history of choking is highly suggestive of foreign body in airways, even if it occurred days or weeks before presentation. The episode may be immediately followed by respiratory symptoms, or there may be a symptom-free period, which must not be misinterpreted as a sign of resolution since it may delay the diagnosis. The absence of choking history does not rule out foreign body in airways, since choking events may be unwitnessed or unrecalled. Inability to breath indicates the need for immediate care and examination of the airways.
Signs of complete airway obstructions include squeaky sounds when trying to breathe (stridor), weak and ineffective coughing, respiratory distress, inability to speak and skin, lips and nails turning blue or dusky (cyanosis). patient can also loss consciousness.
Approach to a chocking patient.
Do not interfere with any choking victim who wants to cough or speak. Coughing is the most effective way to clear a foreign body and ability to speak indicates adequate ventilation.
Open Airway, if foreign bodies visible try to remove it. If attempts to remove obstruction are not successful – perform standard cardiopulmonary resuscitation (CPR) with chest compression and rescue breaths. Recheck the foreign body after every – 2 minutes.
NOTE: Do not attempt blind finger sweeps.
If complete obstruction and patient conscious:
>1 year of age
-Abdominal thrusts (Heimlich) or chest thrusts in larger or pregnant patients,
-Continue until obstruction is relieved or patient become unconscious.
Infants (< 1year old) - back slaps or chest thrusts.
Back slaps. Place one arm across the person's chest for support. Bend the person over at the waist so that the upper body is parallel with the ground. Deliver five separate back blows between the person's shoulder blades with the heel of your hand.
Heimlich maneuver.
if rescuer is present; Patient should be awake and upright. While standing behind the patient, place your fist in the center at the upper part of the belly(xiphoid). Pull inward & upward with your fist Repeat until object is dislodged or patient becomes unconscious .
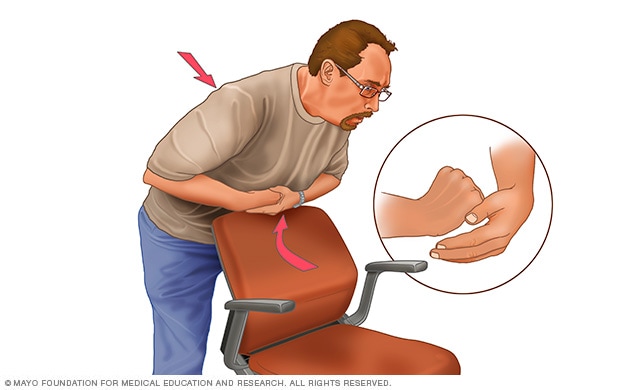
First, if you're alone and choking, call your local emergency number immediately. Then, although you'll be unable to effectively deliver back blows to yourself, you can still perform abdominal thrusts to dislodge the item.
Place a fist slightly above your navel. Grasp your fist with the other hand and bend over a hard surface — a countertop or chair will do. Shove your fist inward and upward.
Incomplete Obstruction + Adequate breathing.
Encourage patient to cough/attempt to remove. Let patient find his/her own comfortable position. Continue with observation/send to hospital if conditions deteriorates.
To clear the airway of an unconscious person:
Lower the person on his or her back onto the floor, arms to the side. Clear the airway. If a blockage is visible at the back of the throat or high in the throat, reach a finger into the mouth and sweep out the cause of the blockage. Don't try a finger sweep if you can't see the object. Be careful not to push the food or object deeper into the airway, which can happen easily in young children.
Begin CPR if the object remains lodged and the person doesn't respond after you take the above measures. The chest compression used in CPR may dislodge the object. Remember to recheck the mouth periodically.




Leave a Comment